The size of the corpus callosum could be a possible biomarker for neurodevelopment in fetuses with congenital heart diseases
Research shows that children with congenital heart defects have a smaller corpus callosum at 32-36 weeks of gestation. BCNatal - Fetal Medicine Research Center, formed by professionals from the Institut de Recerca Sant Joan de Déu (IRSJD) and IDIBAPS, leds this research.
Around 50% of cases of significant congenital heart disease will present, to a greater or lesser extent, a neurodevelopmental disorder that may include cognitive disorders, delayed acquisition of language and motor milestones, attention deficits and behavioral disturbances, among others. These disorders may be evident in early childhood, and their impact extends into adolescence and adulthood. Traditionally, this poor outcome was considered a consequence of alterations in brain development due to the surgery that infants with heart disease undergo. Still, in recent years, many structural brain changes are already present in the prenatal stage.
During fetal life, changes in nutrient supply and oxygen concentration in the brain can generate changes in brain volume, cortical maturation and maturation of the white matter, mainly affecting those fetuses with heart disease with an expected brain flow with lower oxygen concentration.
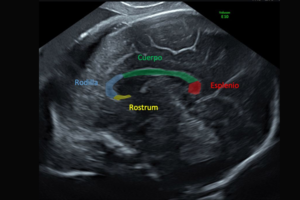
The white matter is the main component of the corpus callosum, the essential cerebral commissure, which communicates the two cerebral hemispheres. The corpus callosum correlates with brain development and maturation. A simple technique such as transvaginal neurosonography measures the corpus callosum volume.
"Previous studies have shown that the corpus callosum size during the fetal period is reduced in fetuses with intrauterine growth restriction or premature parts and is associated with alterations in language acquisition. Until now, it had never been analyzed whether fetuses with major congenital heart disease presented a reduction in the size of the corpus callosum by ultrasound", comments Dr Miriam Pérez-Cruz, researcher of the Environment and complications during pregnancy group (IRSJD).
The article, published in the journal Ultrasound in Obstetrics & Gynecology, has shown that those fetuses with significant congenital heart disease had a smaller corpus callosum in the third trimester of gestation compared to fetuses without pathology, with these differences being more notable in the group of heart disease associated with a more significant reduction of oxygen and nutrient supply to the brain.
"These results confirm an association between the prenatal size of the corpus callosum and neurodevelopment. So the evaluation of the corpus callosum by ultrasound could be an excellent biomarker to identify fetuses at higher risk of presenting neurodevelopmental disorders. Dr. Elisenda Eixarch, a professional at the Hospital Sant Joan de Déu and researcher at IDIBAPS, comments.
The measurement of the corpus callosum could be a simple and handy tool both for clinical practice and for counselling families, especially for implementing personalized and early strategies to improve the neurodevelopment of children affected by congenital heart disease.
All the research has been developed entirely by a team of BCNatal-Fetal Medicine Research Centre, specifically by: Miriam Pérez Cruz, Olga Gómez del Rincón, Mónica Piquer Gibert, Narciso Masoller Casas, María Edda Marimon García, Diana Lip Sosa, Mar Bennassar, Elisenda Bonet Carné, Lola Gómez Roig, Josep Maria Martínez Crespo, Eduard Gratacós Solsona and Elisenda Eixarch Roca.
Reference paper
Pérez-Cruz M, Gómez O, Gibert M, Masoller N, Marimon E, Lip-Sosa D, Bennasar M, Bonet-Carne E, Gómez-Roig MD, Martínez-Crespo JM, Gratacós E, Eixarch E. Corpus callosum size by neurosonography in fetuses with congenital heart defect and relationship with expected pattern of brain oxygen supply. Ultrasound Obstet Gynecol. 2022 Feb;59(2):220-225. doi: 10.1002/uog.23684. Epub 2022 Jan 12. PMID: 33998077.
The measurement of the corpus callosum could be a simple and handy tool both for clinical practice and counseling families.
